People also read this

Last Updated: 24 Mar 2025
CritiShield Plus: The Ultimate Critical Illness Insurance Plan for Complete Coverage & Financial Security
CritiShield Plus: The Ultimate Critical Illness Insurance Plan for Complete Coverage & Financial Security
Written By: Ankita

Last Updated: 10 Mar 2025
International Women’s Day 2025: ‘Accelerate Action’ for a Brighter Future
International Women’s Day 2025: ‘Accelerate Action’ for a Brighter Future
Written By: Ankita
Last Updated: 05 Mar 2025
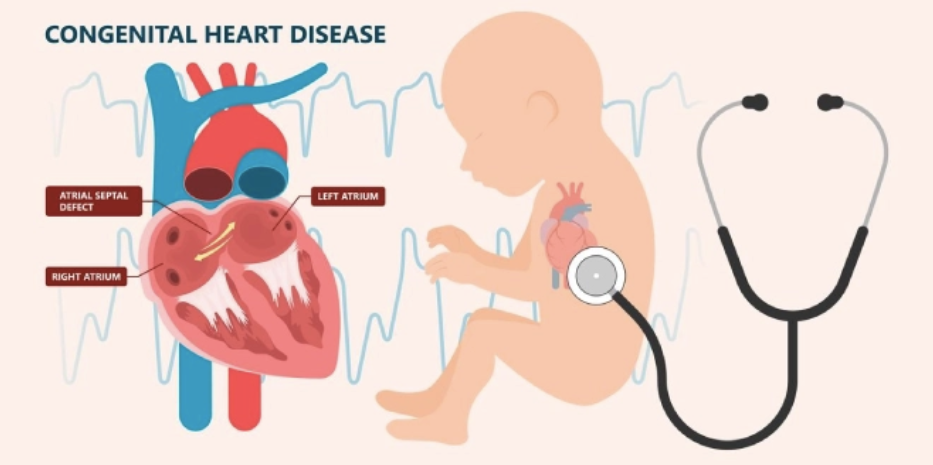
Congenital Heart Diseases: Causes, Prevention, and Awareness for a Healthier Future
Congenital Heart Diseases: Causes, Prevention, and Awareness for a Healthier Future
Written By: Ankita

Last Updated: 05 Mar 2025
Health Insurance Premiums up by 73%, Sum Assured Cover Up by 240% – What’s Driving the Hike post Covid ?
Health Insurance Premiums up by 73%, Sum Assured Cover Up by 240%
Written By: Ankita

